Dental Benefits
Information about your benefits under the NYS Dental Plan administered by Anthem. As of October 1, 2024, Anthem is the plan administrator for the New York State Dental Plan. Your benefits are not changing; please refer to the EmblemHealth Certificate, Attachment, Rider, Non-Participating Provider Reimbursement Schedule and other benefit documents until Anthem branded documents are available in 2025. Click here to learn more about the change.
New York State Dental Plan
Plan Documents
Frequently Asked Questions
Administrator Change to Anthem Blue Cross, effective 10/1/2024
To find out if your current provider participates in the Anthem network, visit https://www.anthembluecross.com/nys-dental.
If you are a NYS Dental Plan enrollee, select "New York State Dental Plan" under Search for a Dental Provider. You will be directed to the XPO Dental Complete – NY State Dental Plan network where you can search for providers by address, doctor name or specialty type.
If you are a NYS Dental Student Employee Health Plan (SEHP) enrollee, select "New York State Dental Plan Student Employee Health Plan (SEHP)" under Search for a Dental Provider. You will be directed to the XPO Dental Complete – NY State Dental Plan SEHP network where you can search for providers by address, doctor name or specialty type. You can filter network results or select "Dental Discount Program Providers" to view providers who may charge you less than their normal fee for services not reimbursed by the NYS Dental SEHP.
There are some situations where a provider may not be listed, so you can also call the dedicated Anthem NYS Dental Plan toll-free number at 1-833-821-1949 to check participating status.
You can complete the NYS Dental Plan Provider Nomination Form available on https://www.anthembluecross.com/nys-dental. The completed form can be submitted to the email address listed on the form.
There will be no impact or changes to your dental benefits as a result of this transition. The benefits outlined in your current New York State (NYS) Dental Plan Certificate of Insurance, Attachment to the NYS Dental Plan Certificate of Insurance and Rider to the NYS Dental Plan Certificate of Insurance and Attachment will not change. Updated Anthem branded documents will be available in 2025. To view your current dental benefit documents, visit the New York State Insurance Plan website at www.cs.ny.gov/employee-benefits. Select New York State Active Employee (NY), your group, Dental and/or Vision and Dental Benefits.
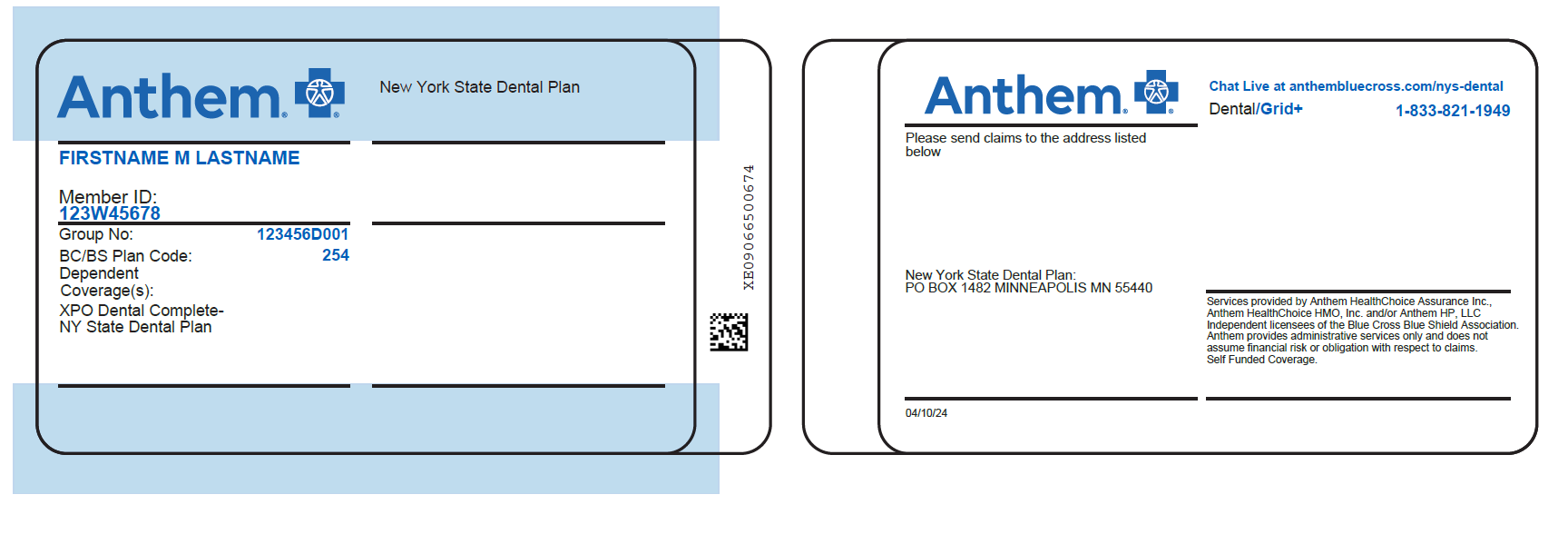
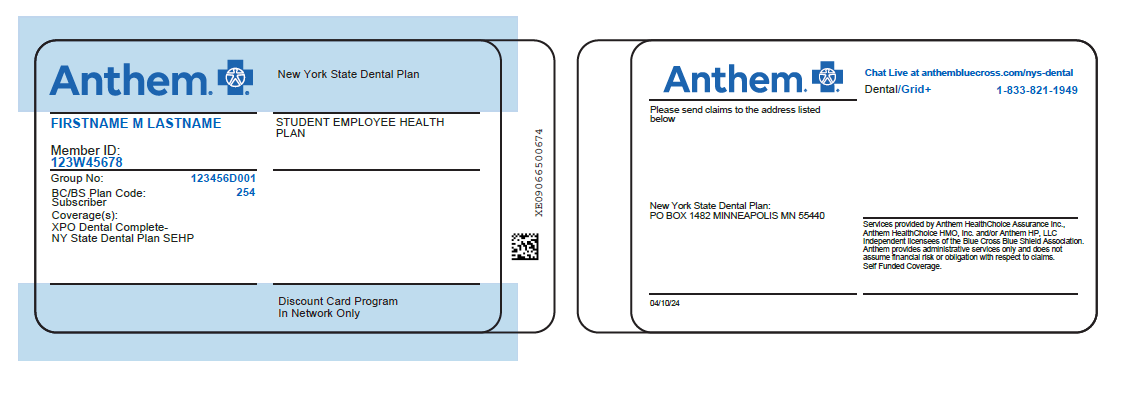
Anthem Blue Cross mailed a welcome letter and a new plan benefit ID card with the Anthem Blue Cross corporate logo in early September. Please note, this was delivered in a safe unmarked envelope to your home address. Beginning October 1, you must use this Anthem ID card when obtaining dental services. If you did not receive your welcome letter and ID card, you can call the dedicated Anthem NYS Dental Plan toll-free number at 1-833-821-1949.
For NYS Enrollees:
For Student Employee Health Plan (SEHP) Enrollees:
If a pre-determination request was submitted to Emblem prior to 10/1/24 and services were approved, Anthem will continue to approve those services 10/1/24 and after. Your cost share could change effective 10/1/24 depending on whether the provider is in-network or out-of- network with Anthem, so you should confirm the participating status of your doctor on https://www.anthembluecross.com/nys-dental or call the dedicated Anthem NYS Dental Plan toll-free number at 1-833-821-1949 with any questions. All services rendered on 10/1/24 and after should be submitted to Anthem either electronically by a participating provider or by mail to: Anthem Dental Claims PO Box 1482 Minneapolis, MN 55440-1482.
Certain restorative, implant, and prosthetic services require multiple visits to complete a course of care and these services may not be billed to insurance until the completion of care. If you started a covered treatment or course of care with an in-network Emblem provider prior to the transition to Anthem on 10/1/24 for these types of services and you receive a bill for the entire course of care at out-of-network charges from the provider post 10/1/24, you can submit your claim to Emblem for consideration as well. The Emblem claim form is available at: https://www.cs.ny.gov/forms/Emblem-Dental-ADA-Claim-Form.pdf.
You will get a denial from Emblem, but then you or your provider have up to 180 calendar days from when you receive the denial to file a Grievance to get your claim considered for payment at the higher, in-network level of benefits. The qualified services must have started before 10/1/24 and completed within 60 days after the Emblem contract termination date. You can file a Grievance by calling Emblem Customer Service at 1-800-947-0101 or by sending your Grievance in writing to: EmblemHealth P.O. Box 12365, Albany NY 12212-2365.
For more information on Grievance and Appeal rights, please reference your NYS Dental Plan Certificate of Insurance on the NYSHIP website or call Emblem Customer Service at 1-800-947-0101 with questions.
Anthem is actively recruiting as many providers into their network as possible. To find out if your current provider participates in the Anthem network, visit https://www.anthembluecross.com/nys-dental and select your Plan name under Search for a Dental Provider. You will be directed to the XPO Dental Complete – NY State Dental Plan network where you can search for providers by address, doctor name or specialty type. There are some situations where a provider may not be listed, so you can also call the dedicated Anthem NYS Dental Plan toll-free number at 1-833-821-1949 to check participating status.
Yes, orthodontia claims with a date of service prior to 10/1/24 will be paid by Emblem. Orthodontia claims with a date of service of 10/1/24 or after will be paid by Anthem. Orthodontia benefits will continue to be paid out monthly.
Is there a video available that will tell me more about the change in NYS Dental Plan Administrator?
Yes. An informational video presentation is available. The approximately 5-minute resource is posted on Anthem's NYS Dental Plan customized website at https://www.anthembluecross.com/nys-dental and on the NYSHIP website under What's New.
Yes. You can securely log-in to the NYS Dental Plan website at https://www.anthembluecross.com/nys-dental. If you currently have active Empire Plan coverage and had previously set up an account with Anthem to view your Hospital Program benefits, you can use your existing username and password. You will be able to view your Hospital Program benefits and your Dental Plan benefits through the same web portal. If you are a new user, you will need your Anthem Dental Plan ID number, which is located on the front of your ID card, to register for an account. Once registered, you will then be able to view your dental benefits and eligibility information.
Anthem also has a Sydney Health mobile app that you can download to your phone or tablet. More information is available at https://www.anthembluecross.com/nys-dental.
Yes, as of October 1, 2024, Anthem offers Direct Pay policies for eligible members. Individuals can enroll at any time on or after October 1, 2024, and coverage will be effective on the first of the month following the date they apply. To find out more about available options, you can visit https://www.anthem.com/ny/individual-and-family/dental-insurance.
You should contact the Employee Benefits Division at 1-800-833-4344. If your COBRA plan has expired, or if you want more information about Anthem's Direct Pay policy for October 1 and after, please go to https://www.anthem.com/ny/individual-and-family/dental-insurance or call the dedicated Anthem NYS Dental Plan toll-free number at 1-833-821-1949.
The dedicated Anthem NYS Dental Plan toll-free number is 1-833-821-1949.
If you are having difficulty finding a participating dental provider near your home address, please reach out to the dedicated Anthem NYS Dental Plan toll-free number at 1-833-821-1949 for assistance.