The Empire Plan is a unique health insurance plan designed especially for public employees in New York State. Empire Plan benefits include inpatient and outpatient hospital coverage, medical/surgical coverage, Centers of Excellence for transplants, infertility and cancer, home care services, equipment and supplies, mental health and substance abuse coverage and prescription drug coverage.

DAVID A. PATERSON
GOVERNOR
DEPARTMENT OF CIVIL SERVICE
ALBANY, NEW YORK 12239
www.cs.ny.gov
NANCY G. GROENWEGEN
COMMISSIONER
NY09-05
TO: State Agency Health Benefits Administrators
FROM: Employee Benefits Division
SUBJECT: Reduced Empire Plan Basic Medical Co-insurance Maximum (OOP)
DATE: January 28, 2009
Effective January 2009, the Reduced Basic Medical Co-insurance Maximum Program, also know as OOP (“Out of Pocket”), has been modified. Previously, the reduced annual basic medical coinsurance maximum was $500 for the enrollee and all covered dependents combined. Effective January, 2009, the reduced annual basic medical coinsurance maximum is calculated in three separate amounts; $300 for the enrollee, $300 for the covered spouse or domestic partner, and $300 for all covered dependent children combined.
The OOP program is extended to Executive Branch Empire Plan enrollees represented by CSEA and DC37, in or equated to salary grade 6 or below, and Judicial Branch employees in or equated to Judicial Grade 6 or below. Eligible employees must be in an Active, Paid Leave or Unpaid Leave status to be eligible for OOP.
NYBEAS PROCESS TO SELECT OOP ELIGIBILITY
During January, EBD will extract the names of eligible employees as of January 1, 2009 based on their grade in NYSTEP and set eligibility. Once eligibility is established, the eligibility flag will be set in NYBEAS, and the enrollees will be moved into different Benefit Programs established for enrollees eligible for this benefit. Benefit Program changes will be processed and sent to the carriers that evening. This Benefit Program change will allow United HealthCare to identify enrollees eligible for this reduced cost and adjudicate their claims accordingly.
Employees who are identified as eligible at the beginning of the year will receive the benefit of the reduced Coinsurance Maximum whenever they are in an eligible bargaining unit during the current plan year. For example, if a person who moves between CSEA and DC37 representation, regardless of changes in grade level, the person will remain eligible for the entire year. However, a CSEA represented person who moves to a PEF represented position would lose the eligibility; because PEF represented employees are not entitled to this benefit. However, if the individual transferred back into a CSEA represented position during the same year, the eligibility for the reduced Coinsurance Maximum would be re-established, regardless of changes in grade level. This will also be true for someone who was terminated and then rehired into a position in an eligible group within the same year.
Going forward, eligibility will be recertified on an annual basis either through NYSTEP for NYSTEP enrolled employees or by the HBAs for non-NYSTEP enrolled and exception employees (see below). The eligibility flag will be reset appropriately at the start of each plan year and Benefit Program changes will be processed and sent to the carriers. The OOP eligibility will always be determined by the employee’s grade level and negotiating unit on January 1 of each year.
Because eligibility is determined as of January 1 of each plan year, a person who is a State employee at the beginning of the year but not eligible based on negotiating unit or grade level will not become eligible during the year. For example, if a current State employee transfers from a noneligible bargaining unit to an eligible bargaining unit or from a grade 7 or above to a grade 6 or below after January 1 of each plan year, that employee will have to wait until the next plan year to become eligible for the benefit.
EMPLOYEES NOT AUTOMATICALLY UPDATED
Those employees who could not be systematically updated for OOP eligibility will be reported through Exception Reports. The Exception Reports are sent to the HBA, who must review eligibility for the benefit with the appropriate Human Resources or payroll staff member.
One or more of the following reports may be sent for review:
- NYBEAS/NYSTEP NON-MATCHING AGENCIES POTENTIAL OOP ELIGIBLE
This report includes employee records for which the agency code in NYBEAS did not match the agency code in NYSTEP.
Example: NYBEAS agency code - 01030 / NYSTEP agency code - 00640
Any employees on leave from a NYSTEP agency who are currently in a non-NYSTEP agency on NYBEAS will show on the report.
- NYSTEP NON-GRADE POTENTIAL OOP ELIGIBLE
This report includes employees from NYSTEP who do not have a valid numeric grade level but may be eligible due to their equivalent salary and or hourly rate. These employees have not been enrolled in the OOP but instead have been reported in this exception report for HBA review of their eligibility. The report includes their compensation rate, pay basis, and job title to assist with determining eligibility.
Example: Grade - NS or OS
- NYBEAS NON-NYSTEP POTENTIAL OOP ELIGIBLE
This report contains the names of employees enrolled in medical benefits from your agency who are not found in NYSTEP. HBAs must determine if the employee is eligible for OOP and if so, manually update the OOP Eligibility page in NYBEAS. In each of the above situations, HBAs will have to review the report(s), determine if the employee is eligible for OOP and if so, update the OOP Eligibility page in NYBEAS (see below). The process described above will be performed annually through 2011 and then end unless the OOP benefit is extended by future negotiated agreements.
OOP ELIGIBILITY TRANSACTION
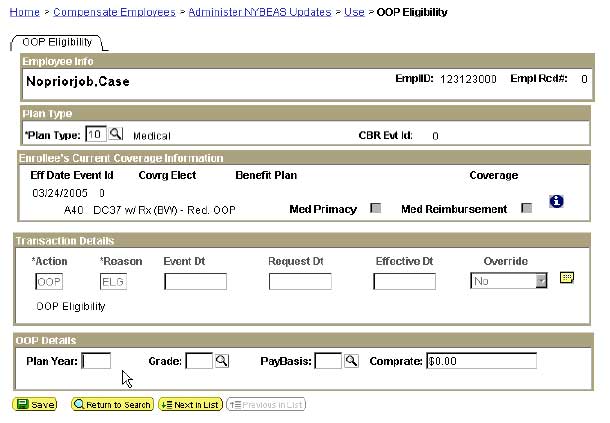
If after review of the above reports, the HBA determines an employee is eligible for OOP, they will need to enter an OOP transaction. To update NYBEAS,
Go to: Compensate Employees > Administer NYBEAS Updates > Use > OOP Eligibility
Enter EmplID and click on the search button
The OOP Eligibility page will appear: Enter Plan Type ‘10’, the ‘Plan Year’ and the Grade. These are all required fields.
Eligible grade levels are 01-06. Current employee eligibility is set at the beginning of the year and the employee remains eligible for the entire year as long as enrolled in an eligible benefit program. (NYBEAS processing of newly hired or rehired employees is discussed below)
Entry of Pay basis Code (“ANN” or “HRY”) is not a required field but may be helpful to the HBA for information purposes in subsequent years.
Enter Comp rate which can be an annual salary or hourly amount (i.e. $25,000 or $9.45). This is not a required field.
OOP ELIGIBILITY PANEL
If the effective date of the OOP enrollment is later than or equal to the first date an enrollee is covered by medical benefits the benefit program will be immediately updated by this transaction.
If the effective date of the OOP enrollment is prior to the first day an enrollee is covered by medical benefits this transaction will create a transaction row that is processed that evening at which time the new benefit program is assigned and all related health, life, and billing rows are carried forward. (This means the HBA will not be able to see the new benefit program until the next day)
*OOP eligibility may be earlier than the top of stack row displayed on the page. An OOP eligibility row will be created and a work list generated for the EBD Corrections Unit to update. The system cannot automatically update due to the blocking dated rows.
See eligibility for new enrollees.
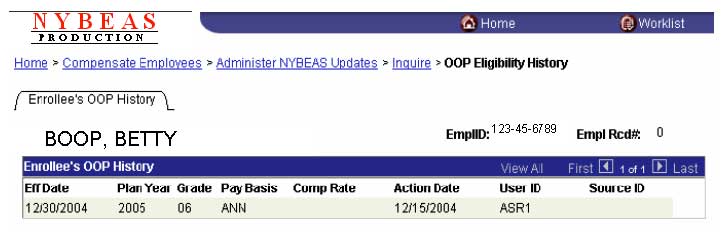
OOP Eligibility History
This page is used to view the history of an enrollee’s OOP eligibility. There will only be one row per year of eligibility status.
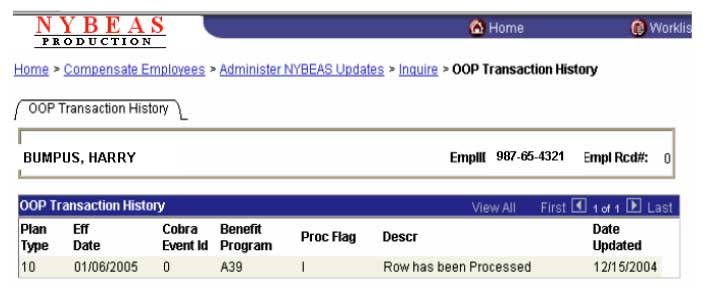
OOP Transaction History
This page is a history of the generated benefit program changes and the process status within NYBEAS and may come from one of these sources: OOP Eligibility Page and Yearly NYSTEP Extract. This is how the page works:
If a Health Benefit or Life Benefit record exists with an effective date earlier than the date of the OOP eligibility then the transaction is written to a table called BEA_OOP_EE_TRAN. The nightly process “OOP Benefit Program Move” is run each night and the enrollee’s records are updated to reflect the change in the Benefit Program. If for any reason the transaction is rejected an error log will be sent to Corrections Unit to take appropriate action. This page will show the results of that process.
Newly Hired or Rehired employees
Employees hired or rehired after the annual OOP update process will not be picked up either systematically or noted on the exception reports discussed above. If the enrollee is assigned a benefit program that is OOP eligible at the time of a medical enrollment, an OOP eligible section pops up at the bottom of the Enroll/Waive screen. At that time the HBA would need to verify the OOP eligibility.
If the employee is eligible, the HBA clicks on the OOP Eligible? Box and enters the appropriate grade level which is required. The OOP plan year automatically fills in based on the effective date entered. Entry of Pay basis Code and Comp rate are optional as discussed above.
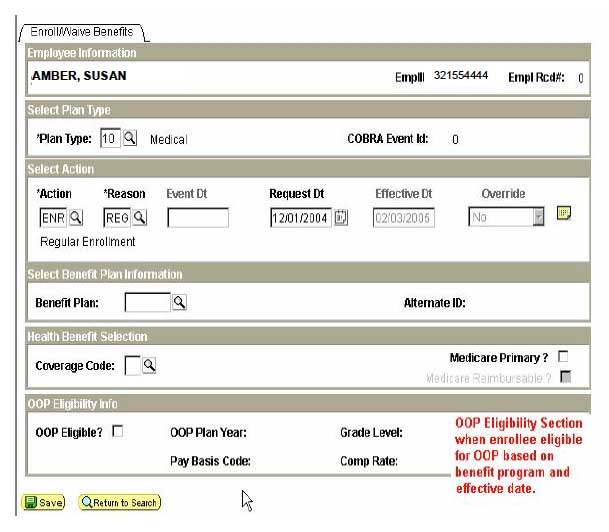
In most cases, the enrollment will update the OOP Benefit Program immediately. In cases where special processing would be required, a Worklist will be created to indicate the benefit program change should be handled manually by EBD Corrections unit staff.
If you have any questions about the OOP program or NYBEAS processing relating to it, please call your processor at the Employee Benefits Division.
