The Empire Plan is a unique health insurance plan designed especially for public employees in New York State. Empire Plan benefits include inpatient and outpatient hospital coverage, medical/surgical coverage, Centers of Excellence for transplants, infertility and cancer, home care services, equipment and supplies, mental health and substance abuse coverage and prescription drug coverage.

PA16-03
PAEX16-03
TO: Health Benefits Administrators of Participating Agencies
FROM: Employee Benefits Division
SUBJECT: 2016 Dependent Eligibility Verification Project
DATE: February 12, 2016
General Guidelines, Timeline and Enrollee Communications
The Department of Civil Service (DCS) has contracted with Health Management Systems, Inc. (HMS) to administer a Dependent Eligibility Verification Audit (DEVA) for 2016. NYSHIP enrollees with family coverage will be required to document the eligibility of their enrolled dependents. Prior to the audit, enrollees were provided the opportunity to remove ineligible dependents without penalty, during a Special Amnesty Period which ended January 29, 2016. Any dependents not removed during the Amnesty Period or children not verified previously during the 2009 Dependent Eligibility Audit, will now be subject to verification.
SPECIAL AMNESTY PERIOD
Special Amnesty Period (Ends January 29, 2016)
The initial phase of the DEVA project was the Special Amnesty Period. During this period, each enrollee with family coverage had the opportunity to remove ineligible dependents. The last day to remove ineligible dependents was January 29, 2016. Forms received after January 29, 2016, will not be processed and those dependents will be included in the Dependent Eligibility Verification Period. All NYSHIP primary dependents reported as ineligible during the Special Amnesty Period will be removed from coverage effective February 1, 2016. Dependents that are Medicare primary will be removed effective April 1, 2016, in accordance with the regulations of the Centers for Medicare and Medicaid Services (CMS).
Mail returned during DEVA Project
Although HMS will be administering the project, maintaining accurate and up-to-date enrollee addresses is the responsibility of the agency HBA. Agencies will be required to update addresses for any enrollees whose correspondence was undeliverable due to an invalid address. To ensure your enrollees receive their Dependent Eligibility Verification Audit communications, EBD has developed a process in which agencies will receive a new worklist when an address update is required. See HBA Worklist (DEVA Invalid address 2016) below, which explains the NYBEAS notification and the procedure to update an enrollee’s address.
HBA Worklist “DEVA Invalid Address 2016”
Agencies are required to attempt to update addresses for enrollees whose DEVA mail was returned with no forwarding address and is therefore, undeliverable. The agency may need to contact enrollees to obtain a new address, if the information is not available. See below for invalid address worklist notification and instructions:
- Access NYBEAS Worklist titled; “DEVA Invalid Address 2016”.
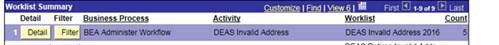
- Click on detail. If the count column shows 1 or more you will need to update the address for the person(s) shown.
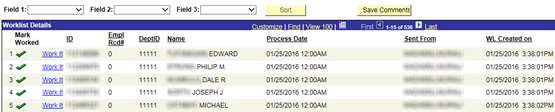
- Enrollees with returned mail will appear as shown below.
- Click on ‘work it’.
- After you click ‘work it’, you will be brought to a new screen that will show the address that the DEVA correspondence was mailed to and returned.
- Once you have obtained the correct address information proceed with processing an address change. (See address change Memo PA 14-22).
- Once the address had been updated, you must access the worklist again to remove the enrollee by selecting the corresponding checkmark in the “Mark worked” column.
Agency Query / Updated Addresses
EBD will process certain address updates automatically from information received from HMS and has developed a new agency query for this process. See Agency Query/Updated Address Information below on how to access this information.
There will be situations when HMS is able to obtain updated address information and provides that information to EBD. When this occurs, EBD will update the enrollee’s address on NYBEAS. Agencies can verify these updates by running a query which will provide a full list of enrollees whose addresses have been updated based on information received by HMS. The query is titled BEA_DEVAUPDATEADR.
Instructions to run a BEA_DEVAUPDATEADR Address Query in NYBEAS: Refer to PA 15-14 memo dated, September 14, 2015.
Dependent Eligibility Verification Period
Now that the Special Amnesty Period has ended, enrollees of Participating Agencies will be required to provide proof of eligibility for dependents during the Verification Period:
February 29 - April 15, 2016
During this time frame, enrollees will be required to submit documentation to verify the eligibility of each of their dependents covered under NYSHIP as of January 1, 2016. Failure to provide sufficient proof will result in the removal of the dependent from coverage effective January 1, 2016. *Please note that due to federal regulations, Medicare-primary dependents covered under Empire Plan MedicareRx will be removed from coverage on a prospective basis, in compliance with CMS termination guidelines.
Dependents not included in the 2016 Dependent Eligibility Verification Audit are:
- Dependent children who were verified in the 2009 Audit
- Dependent Survivors
- Dependent children covered under a National Medical Support Order (NMSO)
- Dependents removed during 2016 Special Amnesty Period
Dependents Removed in Error during the Amnesty Period:
Enrollees who notify you that a dependent they elected to remove during the Amnesty Period was removed in error will be responsible for providing you with the appropriate verification documents within 30 days of the Amnesty Termination Notice. To re-add the dependent refer to HBA Memo PA 10-15 for required proofs. The dependent will not be included in the DEVA Project and will not be audited by HMS. If documentation is not received within 30 days of the Amnesty Termination Notice, the dependent will be subject to the late enrollment provision.
ENROLLEE COMMUNICATIONS:
Samples of enrollee communications will be posted to the NYSHIP website in the Current Topics section.
Please encourage your enrollees to respond to HMS when they receive their Dependent Eligibility Verification Audit packets. Enrollees may visit HMS’s online web portal at www.verifyOS.com. Through this online web portal, enrollees can check their status, upload verification documents, and link to resources that will help them obtain the required documentation.
CONTINUATION OF COVERAGE (COBRA)
New York State is not offering COBRA to dependents that are removed during the DEVA Project. However, whether to offer COBRA to dependents removed as result of this project is at the discretion of the employer. PA enrollees with questions concerning COBRA will be referred to their employer for this information.
Note: If the dependent is no longer eligible because of a “qualifying event,” (e.g., divorce, child reaches age limit) COBRA, or the Consolidated Omnibus Budget Reconciliation Act, gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances when a timely request is made.
