The Empire Plan is a unique health insurance plan designed especially for public employees in New York State. Empire Plan benefits include inpatient and outpatient hospital coverage, medical/surgical coverage, Centers of Excellence for transplants, infertility and cancer, home care services, equipment and supplies, mental health and substance abuse coverage and prescription drug coverage.

ANDREW M. CUOMO
Governor
LOLA W. BRABHAM
Commissioner
PA20-13
TO: Participating Agency Health Benefit Administrators
FROM: Employee Benefits Division
SUBJECT: Letter Automation Project
DATE: August 17, 2020
The Employee Benefits Division (EBD) is pleased to announce the automation of letters to enrollees in the New York State Health Insurance Program (NYSHIP) when certain transactions are processed in NYBEAS.
A letter will be generated automatically when the following transactions are entered:
- Plan Change – PLN/SPC, PLN/OPN: Changing to/from a NYSHIP HMO, the Empire Plan or Opt-out.
- Dependent Delete – DEP/DEL, DEP/DIV, DEP/DEC, DEP/DPT, DEP/DPV: Removing a dependent from a family policy, where at least one other dependent remains covered.
- Dependent Add – DEP/ADD, DEP/MAR, DEP/NWB, DEP/PCT, DEP/ADP: Adding one or more dependents to an existing family policy.
- Change to Individual – CCO/VOL, CCO/DEC, CCO/DEL, CCO/DIV, CCO/EXT, CCO/OPN, CCO/DPT, CCO/DPV: Changing from a family to an individual policy.
- Change to Family –CCO/MAR, CCO/NWB, CCO/PCT, CCO/REQ, CCO/ADP: Changing from an individual to a family policy.
- Payment Method Change – PMC/DIR, PMC/APY, PMC/ERS, PMC/TRS: Changing the method in which an enrollee is billed for their premiums.
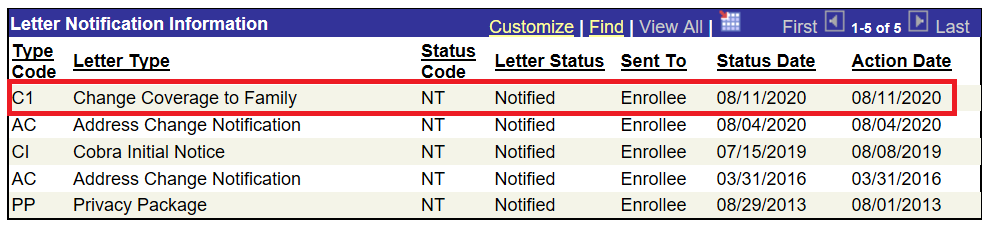
Once the transaction is processed, a letter will be queued for printing that evening and mailed the following business day. You can verify that the letter was generated by viewing the Letter Notification page in NYBEAS. This page can be accessed by visiting Benefits > History > Letter Notification.

A list of letters mailed to the member will be populated along with its current status and process date.
Example:
The following chart catalogues possible Letter Type and Type Code (you may see other Codes and Letters produced by EBD) associated with corresponding transactions:
|
Type Code |
Letter Type |
|
C1 |
Change to family coverage |
|
C2 |
Change to individual coverage |
|
D1 |
Add a dependent |
|
D2 |
Remove a dependent |
|
P1 |
Option change |
|
P2 |
Payment method change |
The Letter Status column indicates which step of the letter generation process the letter is presently in. Possible Letter Status and Status Codes are listed in the following chart:
|
Status Code |
Letter Status |
Definition |
|
NT |
Notified |
The letter was produced. |
|
UN |
Unprocessed |
The letter has not yet been produced but is queued to generate overnight. |
|
NP |
Not Processed |
The letter was not produced. |
Note: Letters posted as Unprocessed (UN) will update the following day to reflect Notified (NT) status. Alternatively, letters in Not Processed (NP) status means EBD updated the record to prevent a letter from being generated for a specific transaction.
Although EBD will mail confirmation letters for these transactions directly to enrollees’ homes, HBAs should continue to notify employees of the change(s) requested and applicable details. This will ensure they are provided with critical information, including changes in premium, which paycheck will be impacted, and whether there will be any retroactivity for billing.
If you have any questions after reviewing this memo, please contact the Employee Benefits Division HBA Help Line at (518) 474-2780. Representatives are available Monday through Friday between 9 a.m. and 4 p.m. Eastern time.
