The Empire Plan is a unique health insurance plan designed especially for public employees in New York State. Empire Plan benefits include inpatient and outpatient hospital coverage, medical/surgical coverage, Centers of Excellence for transplants, infertility and cancer, home care services, equipment and supplies, mental health and substance abuse coverage and prescription drug coverage.
KATHY HOCHUL
Governor
TIMOTHY R. HOGUES
Commissioner
PE25-02
PA25-02
TO: Health Benefits Administrators of Participating Employers (PEs) and Participating Agencies (PAs)
FROM: Employee Benefits Division
SUBJECT: Mandatory Federal Premium Reporting Requirement, Plan Year 2024
DATE: January 29, 2025
As part of the Consolidated Appropriations Act, the federal government has established an annual requirement that all health insurance issuers, employer-based health plans and other group health plans report the average monthly premium paid by employees and the average monthly premium paid by employers. These reporting requirements are outlined in the Prescription Drug Data Collection (RxDC) Reporting Instructions published by the Centers for Medicare and Medicaid Services.
To meet this requirement, the Department of Civil Service must collect 2024 premium contribution information from all Participating Agencies (PAs) and Participating Employers (PEs).
Please complete data entry on the Federal Premium Reporting page in NYBEAS by following the instructions below. This survey is mandatory for all NYSHIP PAs and PEs and must be completed by March 31, 2025.
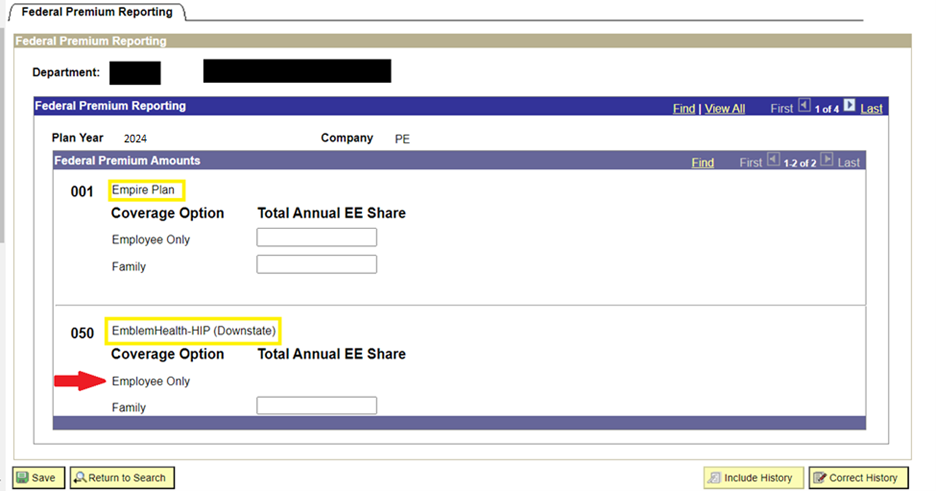
First, sign into NYBEAS and click Benefits. Under the Transactions folder, click Federal Premium Reporting.

Enter your agency code in the Department box and click Search.
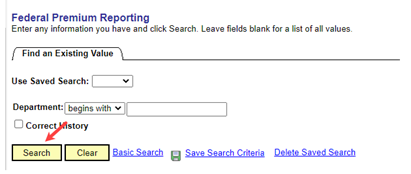
On the new page, enter the total annual EE share (enrollee share) of NYSHIP health insurance premium for each benefit plan (Empire Plan, Excelsior Plan[1] or NYSHIP HMO[2]) and coverage option (Employee Only and Family). Plan year is indicated at the top of the page.
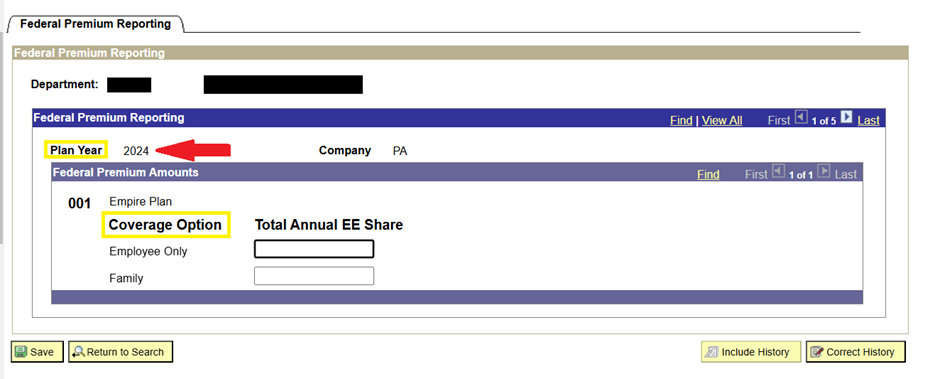
Total annual EE share is the combined dollar amount all employees, retirees, vestees, dependent survivors, COBRA enrollees and Young Adult Option enrollees paid for coverage (regardless of whether they are NYSHIP-primary or Medicare-primary).
It includes amounts your agency or the Employee Benefits Division billed enrollees directly, deducted from enrollees’ pay and deducted from pensions for retirees, vestees and dependent survivors.
If necessary, you can determine if an enrollee’s premiums were paid directly to your agency or deducted from their pension by reviewing the enrollee’s NYBEAS Accounting tab in NYBEAS Update History. If your agency paid 100 percent of the premium for your enrollees, enter $0.01 in that field. (The page will not accept a value of $0.00.
This update in NYBEAS is only for NYSHIP premiums paid by enrollees. Do not enter the amount your agency contributed towards the premium. Do not enter any premium information for non-NYSHIP plans offered by your agency.
If your agency offers different NYSHIP plans, you will need to enter information for each benefit plan and coverage option.
Agencies without enrollees in a certain coverage option will have no box for that option. In the example below, an agency offers both The Empire Plan and EmblemHealth-HIP (Downstate). Because there are no EmblemHealth-HIP (Downstate) enrollees with Employee Only coverage, there is no box for that option. The total annual EE share for Family coverage should still be entered.
This is an annual federal reporting requirement. If you have any questions, contact the HBA Helpline at 518-474-2780.
[1] PA only
[2] PE only
